The menstrual pain-brain connection
Pain is not just a symptom. It's a complex experience deeply influenced by biological, psychological, and social factors. Pain is also notoriously difficult to measure
Pain is not just a symptom. It's a complex experience deeply influenced by biological, psychological, and social factors. Pain is also notoriously difficult to measure - and the most widely adopted tools rely on the subjective reports of sufferers. This approach is inherently flawed, as it rests on the perceived credibility of the person reporting the pain—leading to a historical oversight of women's pain experiences. The gender pain gap serves as a clear testament to this issue. The most common treatment for pain - a chemical painkiller in the form of a pill - also hasn’t evolved much since the 1980s. Yet chronic pain continues to be the most significant and silent epidemic, affecting more than 28 million adults in the UK alone. The medical world finds pain frustrating, if not painful - its indescribability and subjective nature make it particularly difficult to treat. In fact, for decades our framing of pain was linear, and it was thought to be no more than a direct sensory response to a painful physical stimulus. Today we know that pain is far more complex and intricate than this.
Rethinking pain
In recent years, a growing number of scientists have begun finding ways to capture pain in quantifiable ways in order for us to better understand it and its underlying mechanisms. Their findings, especially in the realm of neuroimaging, reveal a complex relationship between pain and the neural networks that process how it is perceived (Davis, 2011). Such research underscores that pain is not just a sensory experience, but also an emotional and cognitive one - and definitely one that varies significantly among individuals (Raja et al., 2021). Neuroimaging has also revealed patterns of similarity between individuals diagnosed with similar pain conditions, allowing researchers to draw connections between brain regions and their role in pain perception (Damascelli et al., 2022).
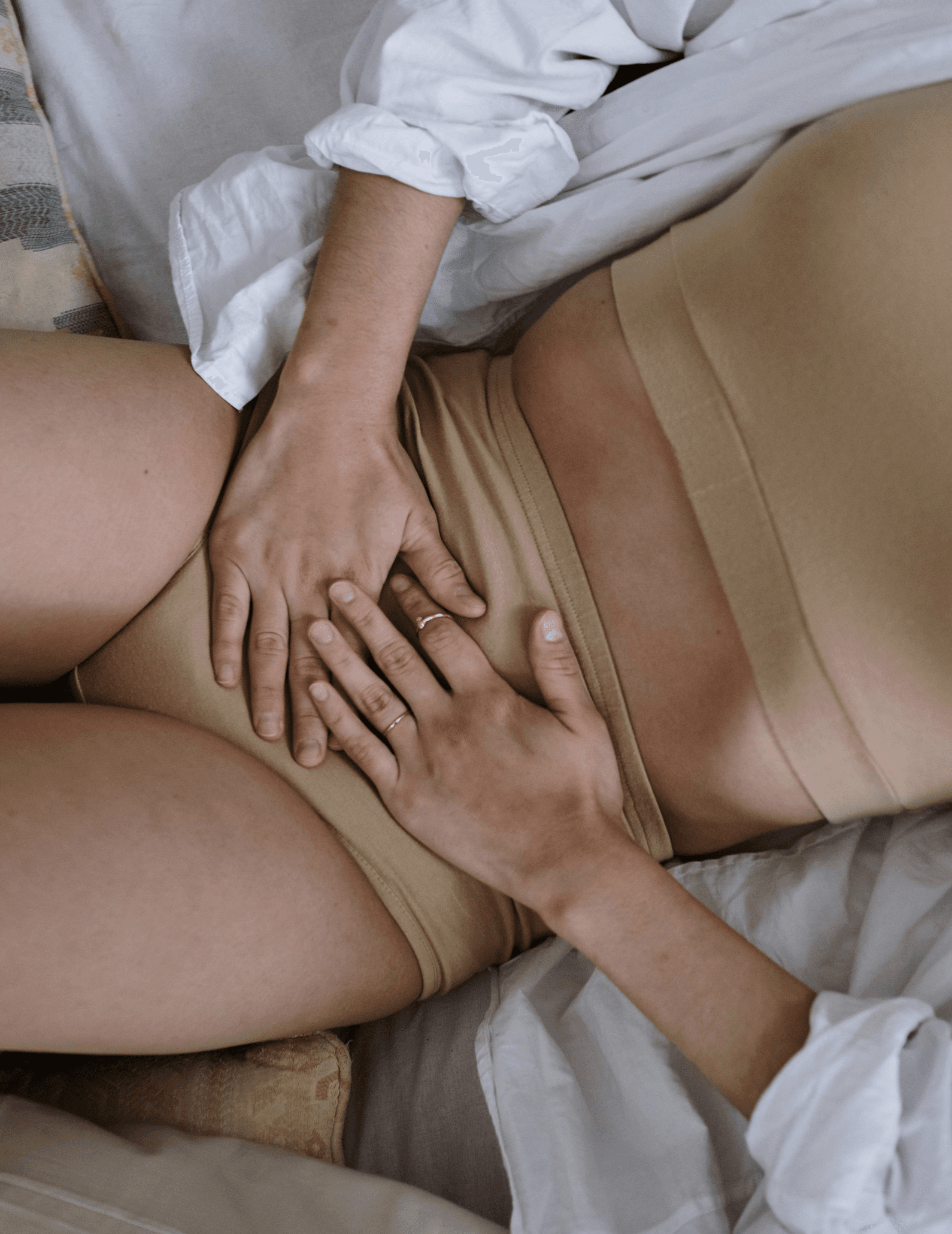
One area where pain research is emerging is in primary dysmenorrhea (PDM), a condition marked by debilitating menstrual pain in the absence of pelvic pathology. Dysmenorrhea is the most common gynaecological condition affecting between 45 to 95% of menstruating women, with studies indicating that at least one in four women will need medication or be absent from study, work or social activities as a result of their pain (Grandi et al., 2012). To give you an idea of how much it affects the quality of life, it’s estimated that the average woman loses 23.2 days of productivity per year as a result of menstrual symptoms (Schoep et al., 2019).
Pain research consistently demonstrates that women with dysmenorrhea exhibit a heightened sensitivity to pain throughout their menstrual cycle, not just during periods of menstrual discomfort but also in phases typically not associated with pain (Iacovides et al., 2015). This increased pain sensitivity, or hyperalgesia, is notable both in areas directly affected by menstrual pain and in muscles not typically involved in menstrual discomfort. These findings are pivotal as they reveal widespread and lasting changes in pain sensitivity among women with dysmenorrhea, lending support to the notion that the condition results in generalized pain sensitization, and thus significantly impacting women's perception of pain.
Primary dysmenorrhea and abnormal brain function
More recent research using neuroimaging helps elucidate the pain-brain relationship in women diagnosed with primary dysmenorrhea. In a study published this year, researchers Yu et. al looked at how brain function changes in women with primary dysmenorrhea by comparing brain scans from 41 women with this condition to 39 healthy women. The study found significant differences in brain connectivity, particularly in areas related to pain and emotion regulation. Specifically, women with primary dysmenorrhea showed increased brain connectivity in regions associated with pain processing and heightened anxiety levels, even when not in pain.
Of particular interest to us are studies that explore the relationship between primary dysmenorrhea and the motor cortex (M1) - which is one of the two key brain regions our neuromodulation device, Nettle™, targets. A 2016 study by Wei et al. delves into the hypothesis that brain networks responsible for pain modulation may function differently in women with primary dysmenorrhea. Using resting-state functional Magnetic Resonance Imaging (MRI), the study investigated the brain's functional connectivity during different menstrual phases, with a particular emphasis on the connectivity between the periaqueductal gray (PAG) and motor areas of the brain in women with dysmenorrhea. The findings indicated increased connectivity between the PAG and motor areas during menstruation but decreased connectivity with the default mode network during the follicular phase, suggesting abnormal or dysfunctional connectivity in the motor region of the brain in individuals with dysmenorrhea.
A 2016 commentary published in Pain Journal supports the theory that the underlying issue in primary dysmenorrhea is not merely inflammation of the uterus but rather an abnormal processing of pain by the central nervous system. The authors claim that this theory is supported by the observed comorbidity between dysmenorrhea and other pain syndromes such as irritable bowel and painful bladder syndrome, suggesting a central sensitization to pain.
The ongoing research around primary dysmenorrhea and brain abnormalities is in line with studies across various chronic pain conditions, which similarly reveal disturbances in the brain's motor region (M1). Moreover, the effectiveness of Motor Cortex Stimulation in treating chronic pain, recognized as a pioneering non-pharmacological intervention, further supports this connection (DosSantos et al., 2016).
Overall, there is a considerable amount of research that suggests that treatments for primary dysmenorrhea might be more effective if they target the central nervous system directly, rather than focusing solely on alleviating inflammation - which is the common approach taken by painkillers. By addressing the root cause of pain processing anomalies in the brain, it's possible not only to reduce the physical symptoms associated with dysmenorrhea but also to mitigate the associated psychological distress, such as anxiety and depression that often accompany this condition (Pakpour et al., 2020). This shift in understanding and treatment approach could significantly improve the quality of life for those affected by primary dysmenorrhea, offering relief that is both more comprehensive and effective.
So, will brain stimulation change how we manage menstrual pain?
We think so. Studies, including those conducted by us, show promising potential of transcranial direct current stimulation in the amelioration of pain. In just one cycle, participants in our double-blind randomised controlled trial experienced a 53% reduction in pain symptoms - an effect likely to improve with sustained use. And unlike traditional treatments such as hormonal contraception and painkillers, brian stimulation offers a non-invasive option with zero severe side effects.
If we begin to reframe pain in relation to the brain and central nervous system, it’s not hard to see that brain stimulation has a theoretical advantage when compared with traditional chronic pain treatments: It directly targets the neural networks involved in pain perception. While advancements in medical technology begin to embrace these discoveries, there is still so much to be done to truly manage pain and its underlying pathologies. Forging new pathways is at the core of our mission at Samphire Neuroscience - and we hope that through developing innovative solutions and investing in research and development, we can unlock neuroscience's full potential for a healthier world.
Related Articles

All about that time of the month
You know what we’re talking about - the days leading up to your period when you often feel low, irritable, and maybe find yourself arguing with your partner more. But what’s really happening?

What your brain is really doing across your cycle
Have you noticed how some weeks you're feeling focused, energetic, and social - while other weeks you feel foggy, tired, and just not yourself? There’s a reason for that, and science finally proves it.
